Rectal Cancer & Robotic Surgery
The location changes everything. The rectum is located in the narrow pelvic basin, surrounded by nerves vital for urinary and sexual function. Dr. Srinivas Bojanapu specializes in Robotic Total Mesorectal Excision (TME), prioritizing "Sphincter Preservation" to avoid a permanent bag whenever oncologically safe. We treat the cancer without compromising your dignity.
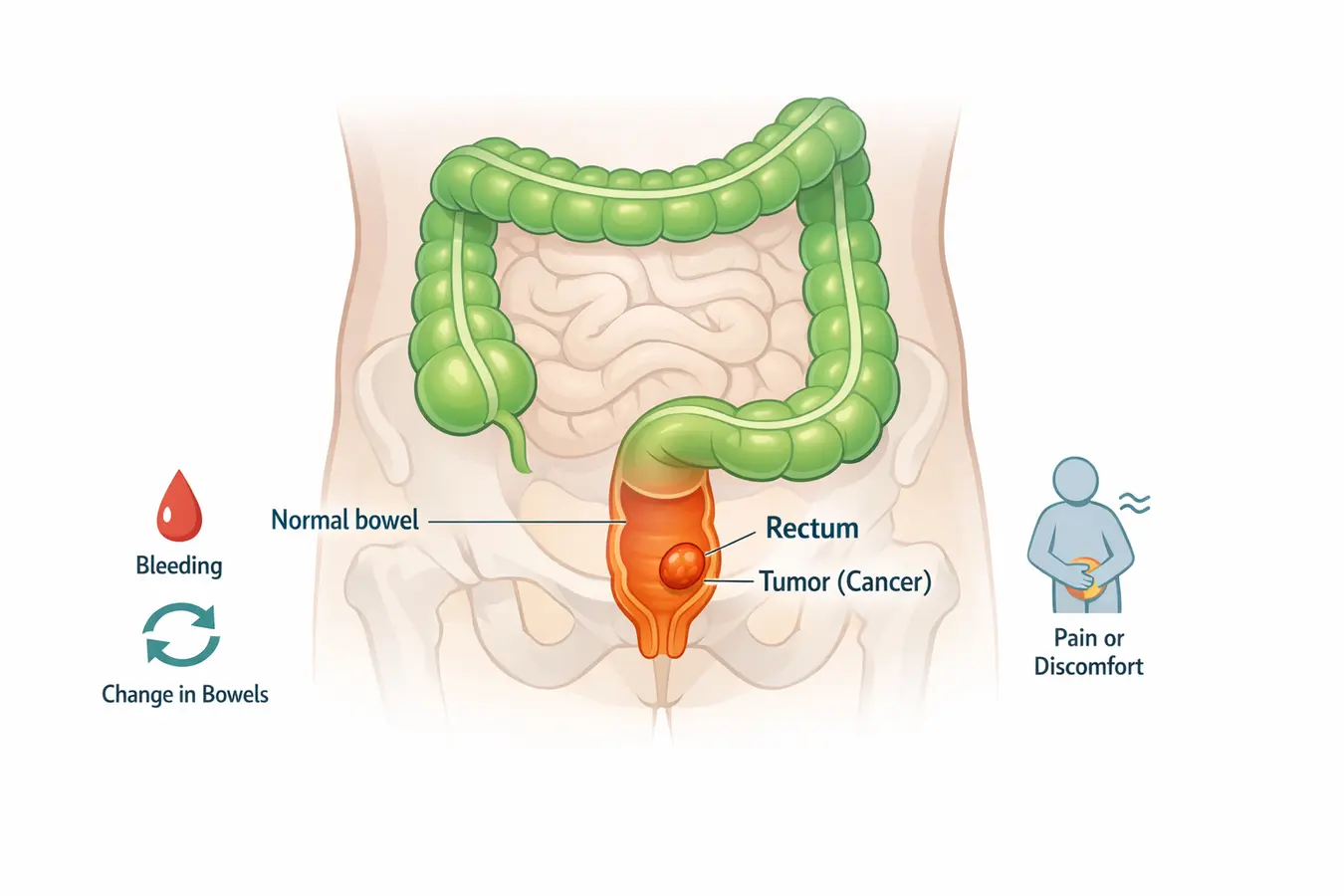
Symptoms & The "Piles" Confusion
⚠️ Critical Note: Rectal cancer is frequently misdiagnosed as Piles (Hemorrhoids) because both cause bleeding. If you have bleeding without pain or a change in bowel habits, you need a specialist exam, not just ointments.
We are seeing Rectal Cancer in younger patients (30-50 years). Do not ignore these signs:
- Altered Bowel Habits: Constipation alternating with diarrhea for >2 weeks.
- Tenesmus: A constant urge to pass stool even when the bowel is empty. This happens because the tumor mimics stool in the rectum.
- Narrow Stools: Stools that look "pencil-thin" due to obstruction.
- Bleeding: Fresh bright red blood (unlike colon cancer which presents with dark/black stools).
The Anatomical Challenge & Robotic Solution
The human pelvis is a tight, cone-shaped space. In men, it is even narrower. Conventional open surgery struggles to reach deep into this basin to remove the tumor without damaging surrounding nerves.
Robotic TME: The Gold Standard
Total Mesorectal Excision (TME) is the Holy Grail of rectal cancer surgery. It involves removing the rectum along with its surrounding fatty envelope (mesorectum) intact, like removing a letter inside an envelope.
- 3D High-Definition Vision: We see nerves magnified 10x, allowing us to spare the tiny nerves responsible for bladder and sexual function.
- 7 Degrees of Freedom: The robotic wrist rotates 360 degrees, allowing us to suture deep in the pelvis.
- Ultra-Low Anastomosis: We can join the bowel very close to the anal muscle, saving the natural passage.
Surgical Options Explained
The surgery depends on the tumor's distance from the anal verge (the opening).
| Procedure Name | Tumor Location | Outcome |
|---|---|---|
| Anterior Resection (AR) | Upper Rectum | Tumor removed, colon joined to rectum. No Stoma. |
| Low Anterior Resection (LAR) | Mid Rectum | Colon joined lower down. Often requires a temporary safety bag (Ileostomy) for 6 weeks. |
| Ultra-Low Resection (ULAR) | Very Low Rectum | Technically demanding. We save the sphincter muscles. Temporary bag is mandatory. |
| APR (Abdomino-Perineal Resection) | Invading Anal Muscles | Rarely done today. Only if the sphincter is cancerous. Permanent Stoma bag required. |
