A comprehensive guide to understanding Liver Tumors (HCC) and the curative "Hepatectomy" surgery. Combining precision diagnostics with advanced robotic resection.
Liver cancer, particularly Hepatocellular Carcinoma (HCC), is a complex condition often arising in the setting of chronic liver disease. However, the liver possesses a unique biological "superpower"—the ability to regenerate.
This regenerative capacity allows surgeons like Dr. Srinivas Bojanapu to perform "Curative Resections" (Hepatectomy). By removing the cancerous portion, the remaining healthy liver can grow back to its full functional volume within weeks, offering patients a chance at a cancer-free life.
Safe Removal Limit
Of healthy liver volume#1 Liver Cancer
Primary IndicationRegeneration Time
To full volumeLiver tumors are not all the same. Accurate diagnosis is the first step to a cure. We treat a wide spectrum of liver pathologies:
Not all liver lumps are cancer. Surgery is only recommended for benign tumors if they are large (>10cm), symptomatic, or at risk of rupture.
Mr. Vikram, a 55-year-old with a history of Hepatitis B, was undergoing routine surveillance when a 4cm lesion was spotted in the right lobe of his liver. He had no pain—a common trait of early liver cancer.
We utilized a Triple-Phase CT Scan to map the tumor's blood supply. A "Liver Volumetry" study confirmed that his left liver lobe was large enough to sustain him.
Mr. Vikram underwent a Right Hepatectomy using CUSA (Ultrasonic Dissector) technology to minimize blood loss. He was discharged on Day 6. Six weeks later, scans showed his liver had regenerated to near-normal volume. He remains tumor-free today.
Liver surgery is complex because the surgeon must ensure the Future Liver Remnant (FLR)—the part left behind—is sufficient to sustain life immediately after surgery.
We use 3D software to calculate the exact volume of the liver to be removed vs. the volume remaining. This eliminates guesswork.
A specialized dye test that measures the functional quality of the liver cells, crucial for patients with cirrhosis.
We can perform a procedure called Portal Vein Embolization (PVE). This blocks blood flow to the tumor side, redirecting all nutrients to the healthy side. This forces the healthy liver to grow (hypertrophy) before the main surgery, making the operation safe.
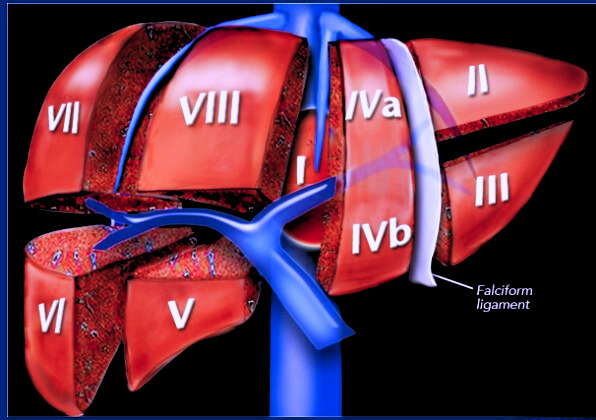
A Hepatectomy involves the precise removal of liver segments based on the Couinaud Classification. This anatomical approach ensures the remaining liver retains intact blood inflow and bile drainage.
The Gold Standard for complex cases.
Ideal for smaller, peripheral tumors.
Reserved for massive tumors.
Recovery is a structured process. Dr. Srinivas and his team follow "ERAS" (Enhanced Recovery After Surgery) protocols to get you back on your feet quickly.
Dr. Srinivas uses the 4th Gen Da Vinci Xi system for minimal scarring, less pain, and faster healing.
Learn about Robotics